Attention Deficit Hyperactivity Disorder or ADHD is a cognitive disorder that afflicts approximately 2-7% of children globally. ADHD prevalence in India, however, is much higher than the global average. As the disorder can affect a person’s everyday functioning even until adulthood, children suffering from ADHD in India stand the risk of long-term negative outcomes such as lower educational and employment attainment.
In terms of social impact, a child with ADHD can cause a lot of anxiety to the people around him, putting strains on parent/sibling-child relationships.
As children with ADHD become adults, they could manifest imbalances in emotion (trouble controlling anger, depression and mood swings, relationships and problems at work) and behavior (getting into addictions and substance abuse, experiencing chronic boredom).
ADHD in India
In India, a study entitled Prevalence of Attention Deficit Hyperactivity Disorder in Primary School Children that was conducted in Coimbatore found ADHD prevalence in children to be higher than the global estimate, at 11.32%. The highest prevalence is found in ages 9 (at 26.4%) and 10 (at 25%).
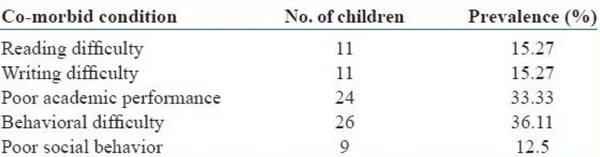
Further, the study showed that more males (66.7%) were found to have ADHD. Children who have ADHD were also observed to not only have poor academic performance and behavioural difficulty but also had problems with reading and writing.
Another ADHD study conducted in different parts of India also suggested a prevalence between 2% to as high as 17%. In numbers, an article published in India Today mentioned that it is estimated that 10 million Indian children are diagnosed with ADHD annually.
What is ADHD?
In the early days, ADHD was also referred to as ‘Attention Deficit Disorder’(ADD). ADD is a milder representation of the symptoms of ADHD - that is without hyperactivity - and is more often seen in girls. Currently, ADD is no longer considered a medical diagnosis and doctors have been using the term ADHD to describe both the hyperactive and inattentive types.
There are 3 types of ADHD.
- Primarily Inattentive
- Primarily hyperactive-impulsive
- Combined
Coping with ADHD
|
While there is presently no cure for ADHD, its symptoms can be managed therapeutically. Thus, it is important for parents to work with their healthcare providers (paediatricians, therapists, etc) and even with schools and teachers to help their children.
Often, ADHD treatment in India involves medication and non-pharmacological interventions. |
 |
Medications
Medicines used to manage ADHD symptoms help to balance and enhance neurotransmitters thereby improving symptoms. Stimulant medicines work for about 70-80% of people. They can be used to treat both moderate and severe symptoms of ADHD.
Some stimulants are approved for children over the age of 3 and children over the age of 6, respectively. These medicines help children, teens, and adults who have a hard time at work, home or school.
Types of medications available for ADHD are:
 |
|
There are other medicines as well. The alternative medicines include Amitriptyline, Bupropion, Escitalopram, Venlafaxine. Doctors may prescribe these for the following reasons:
- If stimulants and non-stimulants don’t work
- If they cause side effects that you can’t live without
- If you have other medical conditions
ADHD Pharmacophobia in Some Indian Communities
|
While ADHD prevalence is quite high in India, parents remain hesitant to subject their children to ADHD drugs. In fact, of those prescribed with ADHD medications, 83.3% discontinue taking their medicines within the first month, a study entitled A preliminary study of factors affecting adherence to medication in clinic children with attention-deficit/hyperactivity disorder, said. Reasons cited by parents for stopping the medication are: side-effects, lack of effectiveness, problems at the hospital, and fear that the child is becoming addicted, among others. Parents, though, especially in the lower-income classes, have shown willingness to tap non-pharmacological methods, a study Hyperactive Around the World? The History of ADHD in Global Perspective, indicated. |
 |
Non-pharmacological solutions | ADHD India
In India, there are alternative solutions being advocated:
- Psychosocial interventions – involve behavioral intervention, parent training, peer and social skills training, and school/classroom‑based intervention/training.
- Body focused - body‑oriented activities such as yoga‑based, physical exercises, sleep and mindfulness‑based interventions such as using breathing exercises with music therapy or attention training.
- Cognitive-behavioral training (such as play therapy).
- Neuro cognitive training - computer-based attention and EEG biofeedback training like the Cogo game launched by Singapore-based Neeuro Pte. Ltd. alongside researchers from the Institute of Mental Health (IMH), the medical school Duke-NUS, and Singapore’s Agency for Science, Technology and Research (A*STAR).
A decade’s worth of work by the researchers suggested that EEG-based attention training is a promising solution. In fact, brain scans done on the children with ADHD in their latest clinical trial, exhibited reorganized brain network activity, meaning having less inattentive symptoms.
Click the banner below to learn more about Neeuro's Cogo solution!






Leave a Comment